Information for people with PANCREATITIS
The following archive information was taken from the PSN charity website which closed in September 2025 and has not been updated since. This information is provided for reference only and should not be considered as a substitute for medical advice.
For up to date information about pancreatitis can be seen on the Pancreas Foundation (hyperlink
https://pancreasfoundation.org/ )
Pancreatitis
What is Pancreatitis?
Pancreas
The pancreas is a large gland behind the stomach and next to the small intestine. The pancreas does two main things
- It releases powerful digestive enzymes into the small intestine to aid the digestion of food.
- It releases the hormones insulin and glucagon into the bloodstream. These hormones help the body control how it uses food for energy.
Pancreatitis is a disease in which the pancreas becomes inflamed. Pancreatic damage happens when the digestive enzymes are activated before they are released into the small intestine and begin attacking the pancreas.
Forms of pancreatitis
There are three main forms of pancreatitis: Acute, Chronic and Cancer of the Pancreas.
Acute pancreatitis
Acute pancreatitis is a sudden inflammation that lasts for a short time. It may range from mild discomfort to a severe, life-threatening illness.
Most people with acute pancreatitis recover completely after getting the right treatment. In severe cases, acute pancreatitis can result in bleeding into the gland, serious tissue damage, infection, and cyst formation. Severe pancreatitis can also harm other vital organs such as the heart, lungs, and kidneys.
Surviving the first acute attack is the most difficult and sadly age does come into this as a major factor. If you are in the later stages of life you are more likely to not survive this first attack as the pain from the attack causes the body to go into shock with major organ failure following.
Chronic pancreatitis
Chronic pancreatitis is long-lasting inflammation of the pancreas. It most often happens after an episode of acute pancreatitis.
Alcohol sensitivity is a major trigger for acute pancreatitis. Those with Chronic pancreatitis must accept they have to live a life of total abstention from any form of alcohol. This could also include mouthwash as it contains alcohol that is absorbed through the cheeks.
Communion wine is another issue as the alcohol sensitivity means you may go days or even years before the accumulative effect of the single drink triggers another possibly fatal attack.
Damage to the pancreas may not cause symptoms for many years, but then the person may suddenly develop severe pancreatitis symptoms.
Pancreatic cancer
The cause of pancreatic cancer is not known, although in the case of ductal-type cancer there is an association with smoking tobacco.
Most commonly cancers of the pancreas arise in the head of the gland. This has two effects.
- First, the cancer blocks the bile duct leading to jaundice, dark urine and pale stools.There is sometimes itching of the skin due to jaundice which rapidly disappears once the blockage is cleared or bypassed.
- Second, the cancer blocks the pancreatic duct leading to poor digestion, loose motions and weight loss. This can be relieved by clearing the blockage or by giving pancreatic enzyme tablets.
Diabetes may already be present in a number of patients prior to developing the cancer or become apparent soon after it is diagnosed or following surgery.
How is it diagnosed?

Ultrasonography
or Ultrasound
This is a simple, painless and relatively quick investigation which can be used to obtain a picture of the inside of the abdomen.
Computerised Tomography
(CT Scan)
This is more complex and time consuming than an ultrasound scan but produces excellent pictures of the pancreas and other abdominal structures.

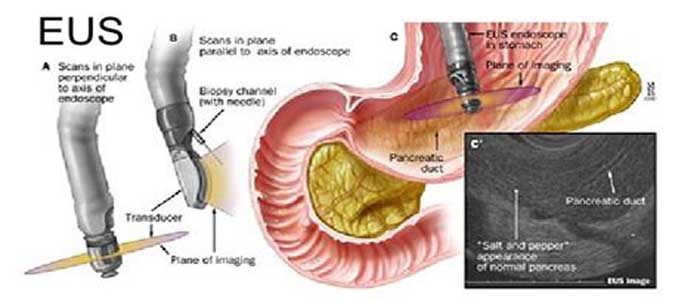
Endoluminal Ultrasound
(EUS)
This is a special investigation for taking ultrasound pictures of the pancreas, pancreatic and bile ducts and surrounding tissue such as blood vessels.
Magnetic Resonance Imaging
MRI scanners use strong magnetic fields, electric field gradients, and radio waves to generate images of the organs in the body.

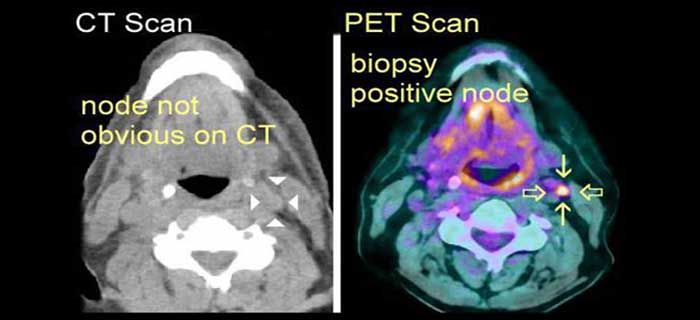
PET Scan
A positron emission tomography is special scan performed in a Nuclear Medicine Department or certain centres if there is uncertainty as to the diagnosis between chronic pancreatitis or a small pancreatic cancer.
Trans-lumbar Approach
Abstract
We (PSN) performed a review of 115 computed tomography guided biopsies of the pancreas done over a 4‑year period to evaluate our experience with the trans lumbar approach to primary pancreatic masses.
The accuracy rate was statistically similar for the transabdominal (87%) and the trans lumbar (90%) approaches. Fewer complications were noted with the trans lumbar approach (0%) than with the transabdominal approach (5%). Overall, we believe that patients experienced less pain with the trans lumbar approach than with the transabdominal approach.
The trans lumbar approach to pancreatic biopsy is a reasonable alternative to the standard transabdominal approach.
Hereditary Pancreatitis
Trypsinogen Gene Mutations
Hereditary Pancreatitis is a rare genetic condition characterized by recurrent episodes of acute pancreatitis attacks. In about half of these cases the problem progresses to chronic pancreatitis, which is severe scarring of the pancreas. Symptoms of an acute attack include abdominal pain, nausea, and vomiting. Laboratory test during an attack usually detect high blood levels of amylase and lipase, which are enzymes released from the pancreas. The first attack typically occurs within the first two decades of life but can begin at any age. In the United States, it is estimated that at least 1,000 individuals are affected with hereditary pancreatitis.
At this time, there is no cure for HP. Treating the symptoms associated with HP is the choice method of medical management. Patients may be prescribed pancreatic enzyme supplements to treat maldigestion, insulin to treat diabetes, analgesics and narcotics to control pain, and lifestyle changes to reduce the risk of pancreatic cancer (for example, NO SMOKING!).
Dietary recommendations to help control pain with digestion include the consumption of small meals throughout the day that are high in carbohydrates and low in protein and fat. Pancreatic enzymes such as Creon, Pancrease, and Violiase are helpful in providing improved digestion and a reduction in diarrhoea and pain for some patients with more advanced disease.
Exposure to smoking and alcohol are known to dramatically increase the risk for pancreatic attacks among individuals with HP. Smoking is strongly discouraged as it doubles the risk for pancreatic cancer. Similarly, alcohol consumption is not recommended for these patients because alcohol is a known risk factor for both acute and chronic pancreatitis. Therefore it is recommended that all HP patients avoid smoking and alcohol consumption.
HP is a genetic disorder, which means that it is usually passed from one generation to the next.
The symptoms of HP are caused by a change to a specific gene. Genes are the packages of information that control how our bodies look and function. A single gene appears to be involved in 60-75% of hereditary pancreatitis families. This gene produces the “cationic trypsinogen” enzyme, which breaks down the proteins present in the foods we eat. (In some research papers cationic trypsinogen is called PRSS1).
When a change to a gene occurs, the gene may no longer function properly. These gene changes are called mutations. Currently, there are two common, and more that 6 uncommon cationic trypsinogen gene mutations that are associated with hereditary pancreatitis. The major mutations are known as cationic trypsinogen “R122H”, “N29I”.
Families with HP might carry one of these mutations, but usually not more than one type of mutation. It is also possible that a family with a strong history of HP may not carry any of the currently known mutations. For this reason, it is believed that additional genes and mutations that cause HP are awaiting discovery. (Every concerned person is encouraged to join ongoing research studies through the University of Pittsburgh 1-888-PITT DNA, or an affiliated medical centre)
HP symptoms can develop at any age, but most patients have their first pancreatic attack before the age of 20. In addition, there is a great deal of variability in the frequency and severity of pancreatic attacks. Some affected relatives may only have a few episodes of pain, while others in the same family experience more severe symptoms. The cause for this variation in symptoms is unknown.
Individuals who have inherited either the R122H or the N29I mutation have an 80% risk of developing clinical symptoms of HP over the course of their lifetime. Although the remaining 20% of these mutation carriers do not show any symptoms, it is important to remember that they still have a risk of having a child who inherits their HP mutation and is affected with HP.
Much less is known about the other mutations, and it is believed that are rare in the population. Without additional knowledge about these mutations, it is not possible to predict how many people will eventually develop symptoms of pancreatitis.
All of our genes come in pairs. We inherit one set of genes from each of our parents. Hereditary pancreatitis is inherited in a dominant manner, which means that only one copy of the HP gene needs to have a mutation in order for an individual to become affected with HP.
When a parent carries an HP mutation in one of their genes, then each child has a 50% (or 1 in 2) chance of inheriting that mutation. It is important to remember that this risk to inherit an HP mutation is 50% for each pregnancy. The risk to have an affected child is actually less than 50% (it is approximately 40%) since one out of five individuals with the R122H or N29I mutation remain symptom-free over their lifetime.
Genetic testing for HP
Genetic testing for HP is currently available both on a research and commercial basis.
Commercial testing is conducted through a licensed laboratory for a specified fee that may be covered by your insurance plan. A small blood sample is drawn at your doctor’s office or hospital laboratory and sent to the commercial laboratory for testing. Results are then provided to your referring physician or counsellor. One commercial laboratory that provides testing for HP is Molecular Diagnostics at the University of Pittsburgh (phone: 412-648-8519). Currently, the fee for commercial testing through Molecular Diagnostics is $276.50 per person. Check with your insurance carrier to determine whether genetic testing is covered by your health plan. Testing can only be done in a laboratory licensed to perform this test. If testing is being done at other institutions within the United States, please call the 888- PITT DNA number to be sure that the site is approved.
Research testing is available for a reduced fee for those who qualify to be enrolled in the HP research study at the University of Pittsburgh. Research testing is confidential, requires the completion of several forms and questionnaires, but may be associated with a longer turnaround period to obtain results.
Genetic testing for any condition is a complex process. Genetic counsellors are available in your local area to help identify the potential risks, benefits, and limitations of genetic testing for HP. Referrals to local genetic counsellors can be obtained from your primary care physician. To find a genetic counsellor near you, ask your physician or call us for assistance at 888-PITT-DNA.
- Individuals who have a relative with a documented diagnosis of hereditary pancreatitis.
- Individuals with a strong history of unexplained abdominal pain that resembles pancreatitis.
See the Genetic Consensus Statement published in Pancreatology 2001;1:405-415, through the Hereditary Pancreatitis Research Study office 888-PITT DNA, or on http://www.pancreas.org/
Before requesting HP genetic test results, we ask that each participant consider the possible benefits and limitations of genetic testing.
Potential benefits of genetic testing:
- Obtaining a diagnosis of HP
Some individuals with HP have reported difficulty in obtaining a diagnosis or explanation of their abdominal symptoms. A positive test result (i.e. when a person is found to carry an HP mutation) may help validate or prove that an individual has true medical symptoms that are hereditary in nature. In short, physicians can use genetic testing to diagnose HP. Identifying relatives at risk to develop HP
Once an HP mutation has been found in a family, other relatives can be tested to determine whether they inherited the same HP mutation. This type of testing, “pre-symptomatic testing,” is conducted for individuals who have not yet developed pancreatitis but are at risk of having inherited an HP mutation from either parent. Individuals who test positive prior to developing symptoms of HP can then be educated about important lifestyle recommendations to reduce the risk of developing future pancreatic disease such as pancreatic cancer. Although pancreatitis cannot be prevented at this time, these individuals would be recommended to avoid the use of tobacco and alcoholic beverages, since these exposures are risk factors for pancreatic cancer in the general population.Reducing feelings such as anxiety or uncertainty
Test results can often help reduce feelings of anxiety and uncertainty for individuals with a family history of HP. For example, an unaffected relative who receives negative test results (i.e. when a person is found NOT to carry an HP mutation) is likely to feel relieved from the uncertainty of whether symptoms will ever develop in the future. Note: negative test results only eliminate the risk to develop a hereditary form of pancreatitis. It is still possible to develop pancreatitis due to other causes later in life.4. Prenatal Genetic Testing. Genetic testing can provide information that is useful when making important reproductive decisions. Prenatal diagnosis is a form of testing that is conducted during pregnancy to determine whether a developing baby has inherited a specific mutation or other health problem. Currently prenatal testing is not being conducted. If both members of the couple have tested negative for a particular HP mutation, then the risk to pass on that HP mutation is essentially zero. For example, if your family is known to carry the R122H* mutation and you test negative for R122H*, then none of your children (or future pregnancies) would be at risk to develop HP.
Potential risks and limitations of genetic testing
Genetic discrimination
As with genetic testing for any type of condition, there is a small but potential threat for insurance and/or employment discrimination. We have never heard of a documented case of this type of discrimination among our research population of over 700 individuals. Moreover, it is reassuring to know that there are no published cases of insurance discrimination with regard to hereditary pancreatitis. Individuals who undergo genetic testing as part of a research study are generally well protected because of our strict rules of confidentiality. For instance, no information about an HP participant is ever released to a third party without written permission from a participant. All blood samples are identified using a code number instead of personal information such as names or social security numbers. Because no research organization can completely eliminate the risk for discrimination, this potential threat should be considered before requesting your genetic test results are confirmed and released to you.Adverse psychological emotions
Powerful emotions such as anxiety, guilt, and depression can accompany the process of genetic testing. In addition, genetic information has a powerful influence on an individual’s reproductive behaviour and a lifelong impact on future descendants.Genetic test results cannot prevent or cure HP
At this time, there is no cure for HP, nor is there a way to prevent pancreatic attacks in patients who carry HP mutations. Furthermore, there does not appear to be a difference in medical treatment for patients who have a hereditary form of pancreatitis versus patients who have a non-hereditary form of pancreatitis.4. “Non-informative” test results.
Non-informative test results include any type of test result that is not conclusive in ruling out a hereditary form of pancreatitis. Negative test results must be interpreted very carefully, especially for individuals undergoing pre-symptomatic testing. Pre-symptomatic testing applied to an individual who is not clinically affected with the disease but has at least one parent affected with a dominant disorder. When test results for now trypsinogen mutations are negative, then . .
If a mutation has been identified in another family member
Interpretation: He/she is not at risk to develop the genetic form of pancreatitis that runs in the family. Since he/she does not carry the mutation, his/her children are not at risk either.
If a mutation has not been identified in another family member
Interpretation: Since we do not know what mutation runs in the family, it is possible that this family carries a mutation that we cannot yet recognize. Therefore it is possible that this person could carry the unrecognizable mutation as well.
Action: Enter a research study with the extended family to search for a new gene mutation.
This information is based on 2001 data for the cationic trypsinogen gene (PRSS1) Disclaimer: This information is intended for general education of individuals who are interested in hereditary pancreatitis and related disorders. It in no way can substitute for the evaluation and care provided to individuals through their trained health care providers. For further information the following publications will be helpful.
Recommended reading (technical)
Chronic Pancreatitis
1. Etemad B, Whitcomb DC. Chronic Pancreatitis: Diagnosis, Classification, and New Genetic Developments. Gastroenterology 2001; 120:682-707. Trypsinogen Gene Mutations The trypsinogen R122H and N29I mutations
2. Whitcomb DC, Gorry MC, Preston RA, Furey W, Sossenheimer MJ, Ulrich CD, et al. Hereditary pancreatitis is caused by a mutation in the cationic trypsinogen gene. Nature Genetics 1996;14(2):141-5.
3. Gorry MC, Gabbaizedeh D, Furey W, Gates LK, Jr., Preston RA, Aston CE, et al. Mutations in the cationic trypsinogen gene are associated with recurrent acute and chronic pancreatitis. Gastroenterology 1997;113(4):1063-8.
4. Whitcomb DC. Hereditary Panceatitis: New insights into acute and chronic pancreatitis. Gut 1999;45:317?22.
5. Whitcomb DC. Genetic Predispositions to Acute and Chronic Pancreatitis. Medical Clinics of North America 2000;84(2):531-47.
Genetic Testing
6. Ellis I, Lerch MM, Whitcomb DC, Committee C. Genetic Testing for Hereditary Pancreatitis: Guidelines for indications, counselling, consent and privacy issues. Pancreatology 2001;1(5):401-11.
7. Applebaum SE, Kant JA, Whitcomb DC, Ellis IH. Genetic testing: counseling, laboratory and regulatory issues and the EUROPAC protocol for ethical research in multi-center studies of inherited pancreatic diseases. Medical Clinics of North America 2000;82(2):575-88.
8. Applebaum SE, OíConnell JA, Aston CE, Whitcomb DC. Motivations and concerns of patients with access to genetic testing for hereditary pancreatitis. American Journal of Gastroenterology 2001;96(5):1610-7.
9. Applebaum-Shapiro SE, Finch R, Pfützer RH, Hepp LA, Gates L, Amann S, et al. Hereditary Pancreatitis in North America: The Pittsburgh – Midwest Multi-Center Pancreatic Study Group Study. Pancreatology 2001;1(5):439-43.
Cancer Risk
10. Lowenfels AB, Maisonneuve P, Whitcomb DC, Lerch MM, DiMagno EP. Cigarette smoking as a risk factor for pancreatic cancer in patients with hereditary pancreatitis. Journal of the American Medical Association 2001;286(2):169-70.
11. Lowenfels AB, Maisonneuve P, Whitcomb DC. Risk factors for cancer in hereditary pancreatitis. International Hereditary Pancreatitis Study Group. Medical Clinics of North America. 2000;84(3):565-73.
12. Lowenfels A, Maisonneuve P, DiMagno E, Elitsur Y, Gates L, Perrault J, et al. Hereditary pancreatitis and the risk of pancreatic cancer. Journal of the National Cancer Institute 1997;89(6):442-6.
SPINK1 Mutations (not discussed in this document)
13. Witt H, Luck W, Hennies HC, Classen M, Kage A, Lass U, et al. Mutations in the gene encoding the serine protease inhibitor, kazal type 1 are associated with chronic pancreatitis. Nature Genetics 2000;25(2):213-6.
14. Pfützer RH, Barmada MM, Brunskil APJ, Finch R, Hart PS, Neoptolemos J, et al. SPINK1/PSTI polymorphisms act as disease modifiers in familial and idiopathic chronic pancreatitis. Gastroenterology 2000; 119:615-23.
15. Whitcomb DC. What to think about SPINK and pancreatitis? Am J Gastrol 2002;(in press).
CFTR Mutations (not discussed in this document)
16. Cohn J, Friedman K, Silverman L, Noone P, Knowles M, Jowell P. CFTR mutations predispose to chronic pancreatitis without cystic fibrosis lung disease (abstract). Gastroenterology 1997;112(4): A434.
17. Cohn JA, Bornstein JD, Jowell PS. Cystic fibrosis mutations and genetic predisposition to idiopathic chronic pancreatitis. Medical Clinics of North America 2000;84(3):621-31.
18. Sharer N, Schwarz M, Malone G, Howarth A, Painter J, Super M, et al. Mutations of the cystic fibrosis gene in patients with chronic pancreatitis. New England Journal of Medicine 1998;339(10):645-52.
19. Noone PG, Zhou Z, Silverman LM, Jowell PS, Knowles MR, Cohn JA. Cystic fibrosis gene mutations and pancreatitis risk: relation to epithelial ion transport and trypsin inhibitor gene mutations. Gastroenterology 2001;121(6):1310-9.
*Note: The trypsinogen R122H and N29I mutations were previously numbered R117H and N21I.
Prepared with the assistance of: Suzanne Applebaum-Shapiro and Laura Hepp and David C Whitcomb MD PhD
Updated: December 18, 2001
